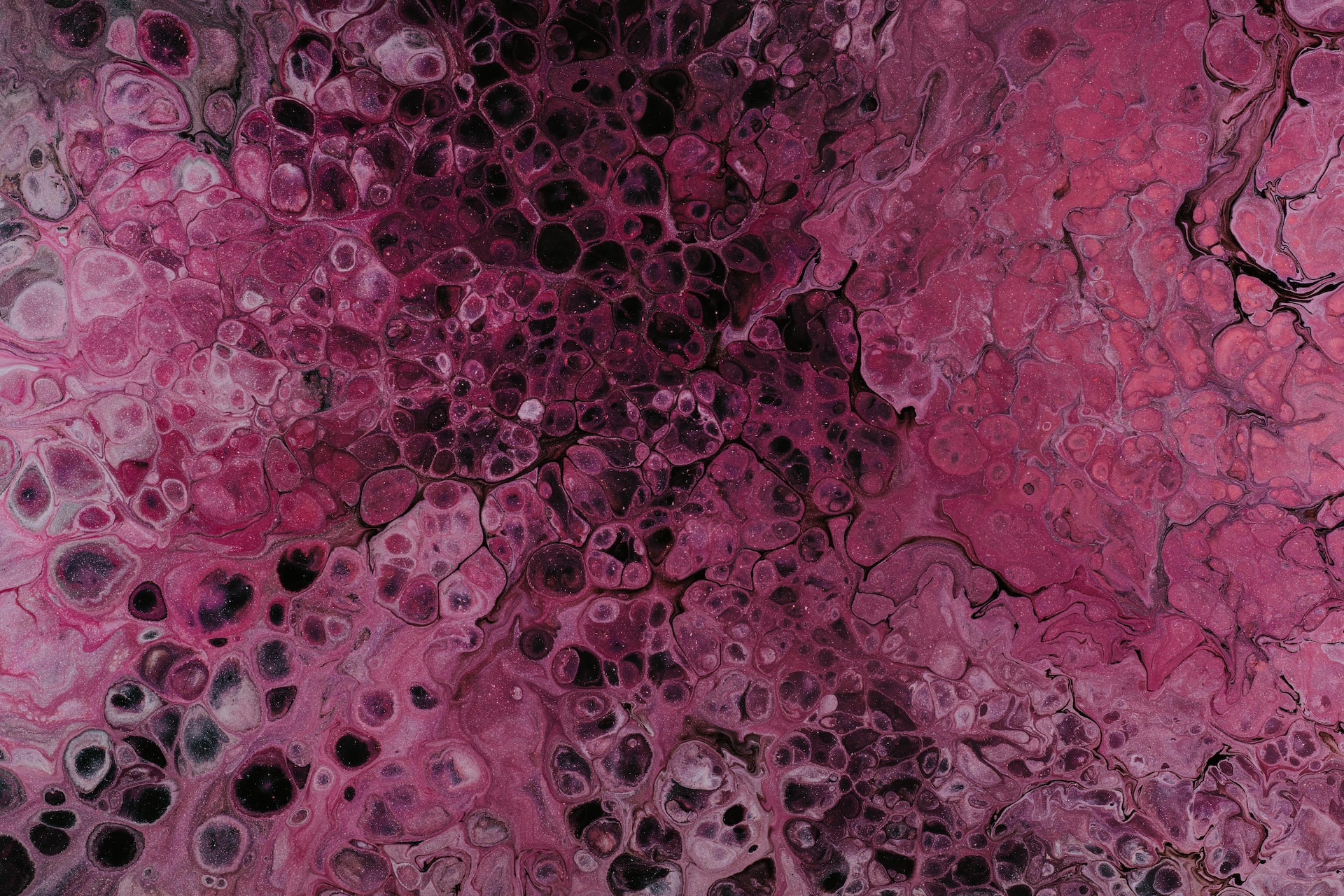
Collagen vascular disease is a term that refers to a group of conditions that affect your connective tissues. Connective tissues are the fibers that provide support and structure to your skin, bones, joints, blood vessels, and organs. Collagen is one of the main types of connective tissue proteins.
Collagen vascular diseases can be classified into two categories: autoimmune and genetic. Autoimmune diseases occur when your immune system mistakenly attacks your healthy tissues, causing inflammation and damage. Genetic diseases are caused by mutations or changes in certain genes that affect the structure or function of your connective tissues.
Types of Collagen Vascular Disease
There are many types of collagen vascular diseases, each with its symptoms and complications. Some of the most common ones are:
-
Lupus
Lupus is a chronic inflammatory disease that can affect any part of your body, such as your skin, joints, kidneys, heart, lungs, brain, and blood cells. Lupus can cause rashes, fatigue, joint pain, fever, mouth ulcers, hair loss, and organ damage. Lupus is more common in women than in men and usually affects people between the ages of 15 and 45.
-
Rheumatoid arthritis
Rheumatoid arthritis is a chronic inflammatory disease that mainly affects your joints, causing pain, stiffness, swelling, and deformity. Rheumatoid arthritis can also affect your eyes, mouth, skin, lungs, heart, blood vessels, and nerves. Rheumatoid arthritis is more common in women than in men and usually affects people between the ages of 30 and 60.
-
Scleroderma
Scleroderma is a chronic inflammatory disease that causes your skin and connective tissues to become hard and thick. Scleroderma can affect your face, hands, feet, and internal organs, such as your lungs, heart, kidneys, and digestive system. Scleroderma can cause skin changes, Raynaud’s phenomenon (a condition where your fingers and toes turn white or blue when exposed to cold or stress), ulcers, breathing problems, heartburn, and kidney failure. Scleroderma is more common in women than in men and usually affects people between the ages of 30 and 50.
-
Sjögren’s syndrome
Sjögren’s syndrome is a chronic inflammatory disease that affects your glands that produce saliva and tears. Sjögren’s syndrome can cause dry eyes, dry mouth, dental problems, fatigue, joint pain, and infections. Sjögren’s syndrome can also affect other parts of your body, such as your lungs, kidneys, liver, pancreas, nerves, and blood vessels. Sjögren’s syndrome is more common in women than in men and usually affects people over the age of 40.
-
Temporal arteritis
Temporal arteritis is a chronic inflammatory disease that affects the arteries in your head and neck. Temporal arteritis can cause headaches, scalp tenderness, jaw pain, vision problems, fever, weight loss, and stroke. Temporal arteritis is more common in women than in men and usually affects people over the age of 50.
-
Ehlers-Danlos syndrome
Ehlers-Danlos syndrome is a genetic disease that affects the production or structure of collagen in your connective tissues. Ehlers-Danlos syndrome can cause hypermobility (excessive flexibility) of your joints, hyperelasticity (stretchiness) of your skin, fragility (easy bruising or tearing) of your tissues, and vascular (blood vessel) problems. Ehlers-Danlos syndrome can affect people of any age or gender.
-
Marfan syndrome
Marfan syndrome is a genetic disease that affects the production or structure of fibrillin-1 (a protein that helps form connective tissue). Marfan syndrome can cause tall stature, long limbs, abnormal curvature of the spine, chest deformity, lens dislocation, heart valve problems, and aortic aneurysm (a bulge in the main artery of your body). Marfan syndrome can affect people of any age or gender.
-
Osteogenesis imperfecta
Osteogenesis imperfecta is a genetic disease that affects the production or structure of collagen in your bones. Osteogenesis imperfecta can cause brittle bones, frequent fractures, short stature, blue sclerae (the whites of your eyes), hearing loss, and dental problems. Osteogenesis imperfecta can affect people of any age or gender.
Causes of Collagen Vascular Disease
The exact causes of collagen vascular diseases are not fully understood. However, some possible factors that may contribute to their development are:
-
Genetic factors
Some collagen vascular diseases are inherited from one or both parents or occur due to spontaneous gene mutations. These diseases are caused by defects in the genes that code for collagen or other connective tissue proteins. These defects can affect the quantity, quality, or function of these proteins, leading to abnormal connective tissue formation and function.
-
Environmental factors
Some collagen vascular diseases are triggered or worsened by exposure to certain environmental factors, such as infections, toxins, drugs, hormones, stress, or sunlight. These factors may cause inflammation or damage to your connective tissues, or alter your immune system’s response to your tissues.
-
Immune system factors
Some collagen vascular diseases are autoimmune diseases, meaning that your immune system mistakenly attacks your healthy tissues as if they were foreign invaders. This can cause inflammation and damage to your connective tissues and organs. The reason why your immune system becomes overactive or misdirected is not clear, but it may involve a combination of genetic and environmental factors.
Diagnosis of Collagen Vascular Disease
The diagnosis of collagen vascular disease can be challenging, as the symptoms and signs can vary widely and overlap with other conditions. To diagnose a collagen vascular disease, your doctor may:
-
Take your medical history
Your doctor will ask you about your symptoms, when they started, how they affect your daily life, and if you have any family history of collagen vascular diseases.
-
Perform a physical examination
Your doctor will examine your skin, joints, eyes, mouth, heart, lungs, and other organs for any signs of inflammation or damage.
-
Order laboratory tests
Your doctor may order blood tests to check for signs of inflammation, such as elevated erythrocyte sedimentation rate (ESR) or C-reactive protein (CRP), or specific antibodies that indicate an autoimmune disease, such as an antinuclear antibody (ANA), rheumatoid factor (RF), anti-double-stranded DNA (anti-dsDNA), anti-centromere antibody (ACA), anti-Scl-70 antibody (anti-topoisomerase I), anti-Ro/SSA antibody, anti-La/SSB antibody, or anti-neutrophil cytoplasmic antibody (ANCA). Your doctor may also order urine tests to check for signs of kidney involvement, such as proteinuria (protein in the urine) or hematuria (blood in the urine).
-
Order imaging tests
Your doctor may order imaging tests to visualize your bones, joints, blood vessels, and organs for any signs of damage or abnormalities. These tests may include X-rays, ultrasound, computed tomography (CT), magnetic resonance imaging (MRI), or angiography.
-
Order biopsy tests
Your doctor may order biopsy tests to obtain a sample of your tissue for microscopic examination. This can help confirm the diagnosis and rule out other causes of your symptoms. The tissue sample may be taken from your skin, muscle, nerve, kidney, lung, or artery.
Treatment of Collagen Vascular Disease
There is no cure for collagen vascular diseases, but treatment can help manage the symptoms and prevent or delay the complications. The treatment of collagen vascular diseases depends on the type and severity of the disease, and may include:
-
Medications
Your doctor may prescribe medications to reduce inflammation, suppress your immune system, relieve pain, prevent infections, or treat specific organ problems. Some of the medications used for collagen vascular diseases are:
- Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or naproxen.
- Corticosteroids, such as prednisone or methylprednisolone.
- Disease-modifying antirheumatic drugs (DMARDs), such as methotrexate or hydroxychloroquine.
- Biologic agents, such as rituximab or infliximab.
- Immunosuppressants, such as azathioprine or cyclophosphamide.
- Anticoagulants, such as warfarin or heparin.
- Antibiotics, antifungals, or antivirals.
- Calcium channel blockers, such as nifedipine or amlodipine.
- Angiotensin-converting enzyme (ACE) inhibitors, such as lisinopril or enalapril.
- Diuretics, such as furosemide or hydrochlorothiazide.
- Beta blockers, such as propranolol or metoprolol.
- Statins, such as atorvastatin or simvastatin.
-
Surgery
Your doctor may recommend surgery to repair or replace damaged organs or tissues. Some of the surgical procedures used for collagen vascular diseases are:
- Joint replacement surgery
- Skin grafting
- Corneal transplantation
- Cataract surgery
- Valve replacement surgery
- Aortic aneurysm repair
Conclusion:
Collagen vascular disease is a term that refers to a group of conditions that affect your connective tissues, which are the fibers that provide support and structure to your skin, bones, joints, blood vessels, and organs. Collagen is one of the main types of connective tissue proteins.
Collagen vascular diseases can be caused by genetic or autoimmune factors or a combination of both. They can affect any part of your body, causing various symptoms and complications. The diagnosis and treatment of collagen vascular diseases can be challenging, but they can help improve your quality of life and prevent further damage.
Collagen vascular diseases are rare but serious conditions that require medical attention and care. If you have any signs or symptoms of collagen vascular disease, you should consult your doctor as soon as possible. Early diagnosis and treatment can make a big difference in your health and well-being.