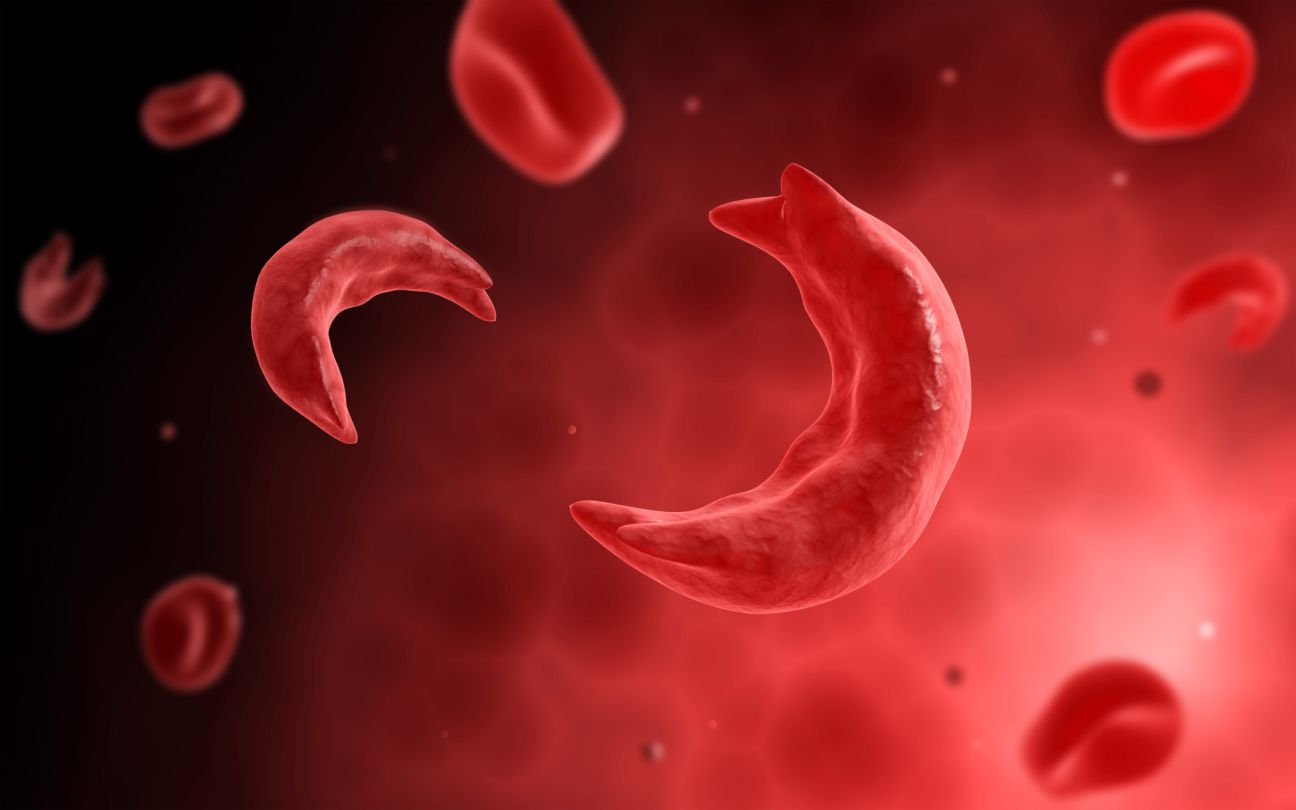
Sickle cell disease (SCD) is a genetic disorder that affects the shape and function of red blood cells. Red blood cells carry oxygen to all parts of the body. People with SCD have red blood cells that are sickle-shaped or crescent-shaped, instead of round and flexible. These sickle cells can block the blood flow in small blood vessels, causing pain and tissue damage. SCD can also cause various complications, such as anemia, infections, organ damage, and reduced life expectancy.
This article will explain the causes, symptoms, diagnosis, treatment, and prevention of SCD. We will also share the latest trends and updates on this condition.
Causes of Sickle Cell Disease
Sickle Cell Disease is caused by a mutation in the gene that makes hemoglobin, the protein in red blood cells that binds oxygen. The mutation changes one amino acid in the beta-globin chain of hemoglobin, resulting in hemoglobin S (HbS). HbS tends to form long, rigid, and sticky fibers when it loses oxygen, which makes the red blood cells sickle-shaped.
SCD is inherited from both parents, who must each carry one copy of the mutated gene. People who have only one copy of the gene are called carriers or have sickle cell trait. They usually do not have symptoms, but they can pass the gene to their children.
SCD is common among people whose ancestors come from sub-Saharan Africa, India, Saudi Arabia, and Mediterranean countries. This is because the sickle cell trait confers some resistance to malaria, a disease that is prevalent in these regions. However, SCD can affect people of any race or ethnicity.
Symptoms of Sickle Cell Disease
The symptoms of Sickle Cell Disease vary from person to person and may change over time. Some of the common symptoms include:
- Anemia: Sickle cells die faster than normal red blood cells, causing a shortage of oxygen in the body. This can lead to fatigue, weakness, shortness of breath, and pale skin.
- Pain crises: Sickle cells can block the blood flow in various parts of the body, causing sudden and severe pain. The pain can last from a few hours to a few days and can affect the chest, abdomen, joints, bones, or muscles. The frequency and severity of pain crises vary among individuals. Some people may have only a few pain crises a year, while others may have more than a dozen.
- Swelling of hands and feet: Sickle cells can block the blood flow in the hands and feet, causing them to swell and hurt. This is more common in babies and young children.
- Infections: Sickle cells can damage the spleen, an organ that helps fight infections. This makes people with SCD more prone to infections, especially by bacteria. Some of the common infections include pneumonia, meningitis, osteomyelitis, and sepsis. Infections can be life-threatening if not treated promptly.
- Delayed growth and puberty: Sickle cells can affect the growth and development of children and adolescents. They may have lower height and weight than their peers and may reach puberty later than normal.
- Vision problems: Sickle cells can block the blood flow in the eyes, damaging the retina, the part of the eye that processes visual images. This can cause blurred vision, floaters, flashes, or even blindness.
- Organ damage: Sickle cells can damage various organs in the body, such as the kidneys, liver, spleen, heart, lungs, and brain. This can lead to complications such as kidney failure, liver cirrhosis, gallstones, heart failure, pulmonary hypertension, stroke, and cognitive impairment.
Diagnosis of Sickle Cell Disease
Sickle Cell Disease can be diagnosed by a blood test that measures the type and amount of hemoglobin in the red blood cells. The blood test can be done at any age, but it is usually done at birth as part of the newborn screening program. The blood test can also be done during pregnancy to check if the baby has SCD or sickle cell trait. The diagnosis of SCD can be confirmed by a genetic test that identifies the mutation in the hemoglobin gene.
Treatment of Sickle Cell Disease
The treatment of Sickle Cell Disease aims to relieve the symptoms, prevent complications, and improve the quality of life of people with SCD. The treatment may include:
- Medications: Several medications can help people with SCD, such as:
- Painkillers: These can reduce the pain during crises or chronic pain. Examples include ibuprofen, acetaminophen, and opioids.
- Hydroxyurea: This is a drug that can increase the production of fetal hemoglobin, a type of hemoglobin that does not sickle. This can reduce the frequency and severity of pain crises and other complications. Hydroxyurea can also lower the risk of infections and stroke.
- L-glutamine: This amino acid can help protect the red blood cells from oxidative stress, which can trigger sickling. This can reduce the number of pain crises and hospitalizations.
- Crizanlizumab: This is a monoclonal antibody that can prevent the sickle cells from sticking to the blood vessel walls, which can cause vaso-occlusion. This can reduce the frequency of pain crises and improve blood flow.
- Voxelotor: This is a drug that can increase the affinity of hemoglobin for oxygen, which can prevent sickling. This can improve the anemia and reduce the hemolysis.
- Blood transfusions: These can provide healthy red blood cells to replace the sickle cells, which can improve oxygen delivery and prevent or treat some complications, such as stroke, acute chest syndrome, or severe anemia. Blood transfusions can be given regularly or as needed, depending on the condition and the risk of complications. However, blood transfusions can also cause side effects, such as iron overload, alloimmunization, or infections.
- Bone marrow transplantation: This is a procedure that can replace the bone marrow, the source of blood cells, with healthy bone marrow from a donor. This can cure SCD, as the new bone marrow can produce normal hemoglobin and red blood cells. However, bone marrow transplantation is not widely available, and it has some risks, such as graft-versus-host disease, rejection, or infections. Therefore, it is usually reserved for people with severe SCD who have a matched sibling donor.
- Gene therapy: This is a novel approach that can correct the mutation in the hemoglobin gene or introduce a new gene that can produce normal or modified hemoglobin. This can potentially cure SCD, as gene therapy can restore the normal function of the red blood cells. However, gene therapy is still experimental, and it has some challenges, such as safety, efficacy, accessibility, and affordability.
Prevention of Sickle Cell Disease
Sickle Cell Disease can be prevented by avoiding the inheritance of the mutated gene from both parents. This can be done by:
- Genetic counseling: This is a service that can provide information and guidance to people who have SCD or sickle cell trait, or who have a family history of SCD. Genetic counselors can help people understand the risk of passing the gene to their children, and the options for prenatal testing, preimplantation genetic diagnosis, or contraception.
- Prenatal testing: This is a test that can detect if the baby has SCD or sickle cell trait before birth. Prenatal testing can be done by analyzing the baby’s DNA from the mother’s blood, the amniotic fluid, or the placenta. Prenatal testing can help parents make informed decisions about their pregnancy and prepare for the care of the baby.
- Preimplantation genetic diagnosis: This is a technique that can select embryos that do not have SCD or sickle cell trait before implanting them in the uterus. Preimplantation genetic diagnosis can be done by using in vitro fertilization (IVF), which involves creating embryos from the eggs and sperm of the parents or donors and testing them for hemoglobin gene mutation. A preimplantation genetic diagnosis can help parents have a baby without SCD or sickle cell trait.
Latest Trends and Updates on Sickle Cell Disease
Sickle Cell Disease is a condition that has been receiving more attention and research in recent years, leading to discoveries and developments. Some of the latest trends and updates on SCD include:
- New medications: In addition to the existing medications, several new drugs are being developed or tested for SCD, such as:
- Rivipansel: This is a drug that can block the activation of a molecule called P-selectin, which is involved in the adhesion of sickle cells to the blood vessel walls. This can reduce the vaso-occlusion and the pain crises.
- Olinciguat: This is a drug that can activate a molecule called soluble guanylate cyclase, which is involved in the relaxation of the blood vessel walls. This can improve the blood flow and the oxygen delivery.
- FT-4202: This is a drug that can activate a molecule called pyruvate kinase, which is involved in the metabolism of red blood cells. This can increase the production of ATP, a molecule that provides energy and prevents sickling.
- IMR-687: This is a drug that can inhibit a molecule called phosphodiesterase 9, which is involved in the degradation of cyclic GMP, a molecule that regulates the production of fetal hemoglobin. This can increase the level of fetal hemoglobin and reduce the sickling.
- New gene therapies: In addition to the existing gene therapies, several new gene therapies are being developed or tested for SCD, such as:
- Lentiglobin: This is a gene therapy that uses a modified virus to deliver a new gene that can produce a modified hemoglobin, called HbAT87Q, which does not sickle. This can replace the defective hemoglobin and restore the normal shape and function of the red blood cells.
- BCL11A enhancer: This is a gene therapy that uses a gene-editing tool called CRISPR-Cas9 to disrupt a DNA sequence that controls the expression of a gene called BCL11A, which is involved in the suppression of fetal hemoglobin. This can increase the level of fetal hemoglobin and reduce the sickling.
- HbGAGT: This is a gene therapy that uses a modified virus to deliver a new gene that can produce a modified hemoglobin, called HbGAGT, which has a higher affinity for oxygen and does not sickle. This can replace the defective hemoglobin and restore the normal shape and function of the red blood cells.
- New clinical trials: Several ongoing or planned clinical trials aim to test the safety and efficacy of new or existing treatments for SCD, such as:
- STRIVE: This is a phase 3 clinical trial that is testing the efficacy and safety of crizanlizumab in reducing the frequency of pain crises in people with SCD who have a history of frequent pain crises.
- HOPE: This is a phase 3 clinical trial that is testing the efficacy and safety of voxelotor in improving anemia and reducing hemolysis in people with SCD who have moderate to severe anemia.
- HGB-206: This is a phase 1/2 clinical trial that is testing the safety and efficacy of lentiglobin in increasing the production of HbAT87Q and reducing the complications of SCD in people with severe SCD who have a matched sibling donor.
- HGB-210: This is a phase 3 clinical trial that is testing the safety and efficacy of lentiglobin in increasing the production of HbAT87Q and reducing the complications of SCD in people with severe SCD who do not have a matched sibling donor.
- HGB-212: This is a phase 3 clinical trial that is testing the safety and efficacy of lentiglobin in increasing the production of HbAT87Q and reducing the complications of SCD in children with severe SCD who have a matched sibling donor.
Conclusion
Sickle Cell Disease is a serious and complex condition that affects millions of people around the world. It can cause various symptoms and complications that can impair the quality and length of life of people with SCD. However, there are many treatments and preventive measures that can help people with SCD manage their condition and live better lives. Moreover, many new developments and innovations are advancing the understanding and treatment of SCD. Therefore, there is hope and optimism for the future of people with SCD and their families.
Check out more articles!